Related topics:
- The dose matters. What are CWF risks to infants?
- Fluorosis, where is the benefit in the risk?
- Research from personal testimony
- References
- LB147 Removing the fluoride mandate – watch the HHS Committee hearing
- Federal Court Rules Fluoridation Poses An “Unreasonable Risk”
- Community water fluoridation news and links
- Community Water Fluoridation in Nebraska
City of Lincoln drinking water update
“Regarding the cautionary statement, we did seek guidance from the Lincoln-Lancaster County Board of Health on this item which was discussed at their February 11th meeting. At that meeting, it was recommended that a statement was not necessary based on the most current research and fluoride policy recommendations by the American Academy of Pediatric Dentistry and the American Academy of Pediatric Physicians. Accordingly, this statement was not included in the 2024 water quality report.” This was the response I received from the City of Lincoln Transportation and Utilities, last Friday, to my request to add a cautionary note to the annual water quality report addressing fluoride risks to infants from community water fluoridation (CWF). The Health Department provided references for their recommendation.(2)(4)
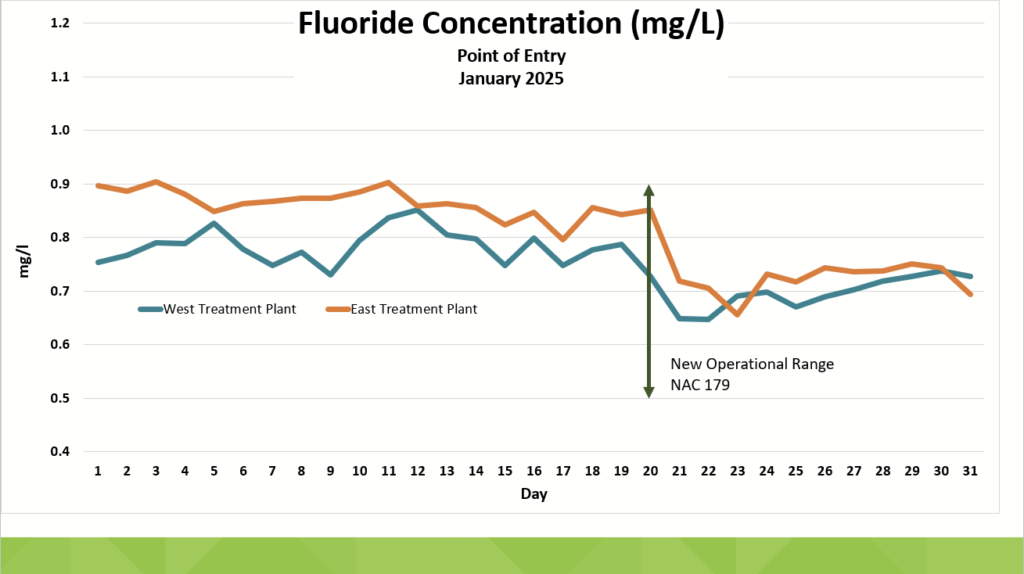
The Health Board’s decision came after several requests were denied for the City and County to reduce the drinking water fluoride treatment level. Unlike MUD-Omaha, Lincoln had been treating its water to a fluoride level of 0.88 parts per million (ppm or mg/L) for years without regard to Nebraska Department of Environment & Energy (NDEE) guidance.
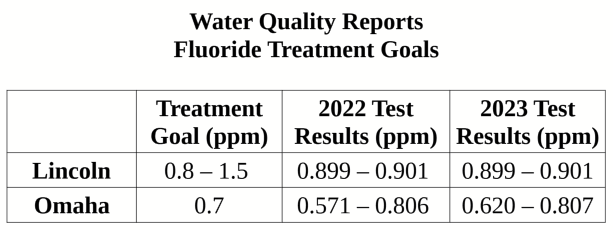
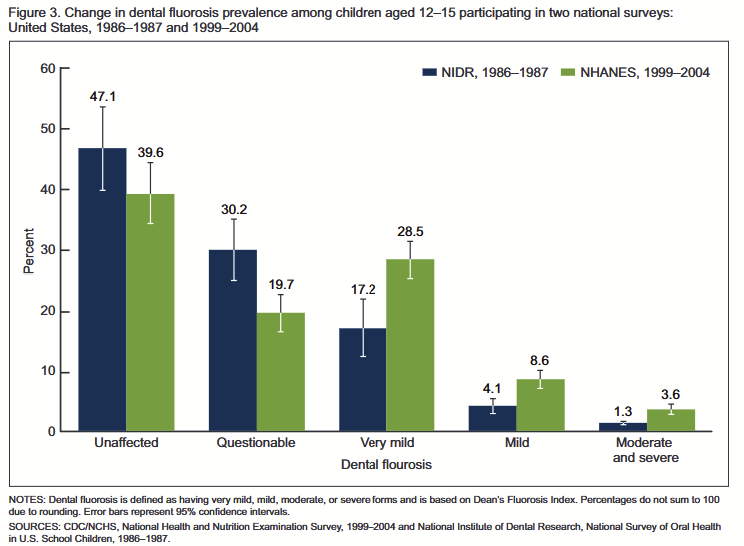
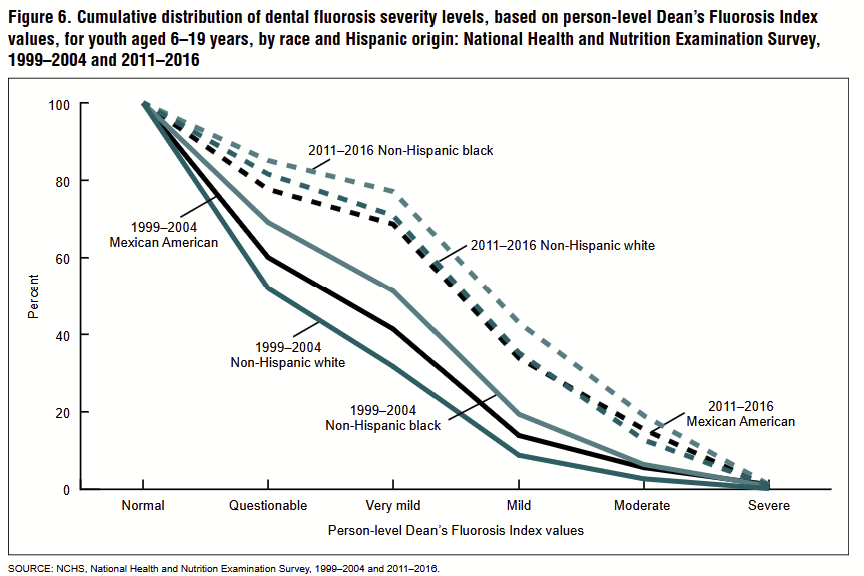
NDEE provided fluoride level guidance because the Nebraska Department of Health and Human Services (DHHS) hadn’t updated its fluoride dosing regulation since 1983 despite the 2011 draft and 2015 final US Public Health Service (USPHS & CDC) recommendation to lower the fluoride level to 0.7 ppm due to rising fluorosis concerns, from 40% to 70%. The DHHS regulation remained between 0.8 and 1.5 ppm until January of this year. DHHS fluoride treatment revisions followed a 2024 petition to update the regulation. In comparison, 68% of water systems nation-wide using systemic dosing reduced fluoride to 0.7 ppm within six months of the 2011 draft issue.
Lincoln’s naturally occurring fluoride level is 0.4 ppm. Lincoln will spend $116,000 this year adding approximately 0.3 ppm of the cheapest fluoride additive, hydro-fluorosilicic acid, a pollution collection byproduct, that offsets industry hazardous waste disposal costs.
What are CWF risks to infants?
“Remember the dose matters…“
Dr. Ann Anderson Berry, MD, LB147 testimony
According to the CDC, infants are particularly vulnerable to chemical exposure because they consume more food and water relative to their body weight compared to adults, leading to higher absorption rates of toxicants. This increased vulnerability is especially critical during the first few months of life when their growth and development are rapid. According to the American Dental Association (ADA), “Reducing fluoride intake from reconstituted infant formula alone will not eliminate the risk of fluorosis development.”(1)
Lincoln’s 2024 Annual Drinking Water Quality Report cautions that, “Some people may be more vulnerable to contaminants in drinking water. This includes… infants. …caregivers should seek advice about drinking water from their health care providers.”
AP SECTION ON ORAL HEALTH. Fluoride Use in Caries Prevention in the Primary Care Setting. Pediatrics. Page 6. Link retrieved 3/28/2025
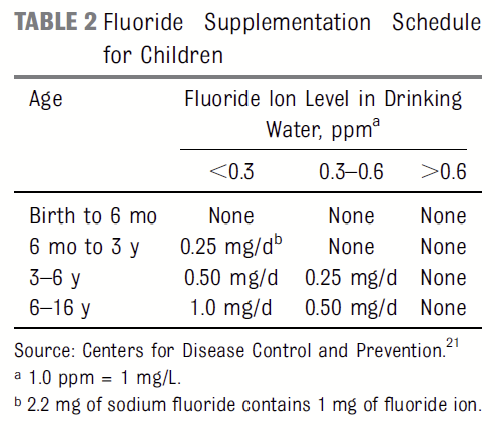
The American Academy of Pediatrics (AAP) recommends no fluoride supplement for infants 0 to 6 months old (Table 2) and advocates for breast milk, as it has consistently low fluoride levels (0.005-0.01 ppm).(1)(2)
“We don’t think that infants between 0 and 6 months of age need extra [fluoride] outside of what they would get in breast milk“
Ann Anderson Berry, MD
The American Academy of Pediatrics also provides risk information on their website HealthyChildren.org saying, “Babies under 6 months old should not get fluoride supplements. After that time, however, breastfed and formula-fed infants need appropriate fluoride supplementation if local drinking water contains less than 0.3 parts per million (ppm) of fluoride.”(5)
Fluorosis, where is the benefit in the risk?
Fluorosis is one of the first visible signs of fluoride toxicity. It is a condition where fluoride causes discoloration of teeth, ranging from white spots to brown stains. Fluoride weakens tooth enamel beginning with very minor changes and progressing to brittleness and pitting with increased and/or prolonged exposure.
Stages of fluorosis

Paradoxically, the ADA claims that mild to moderate fluorosis is merely cosmetic and that fluoride helps rebuild (remineralize) weakened tooth enamel and can reverse early signs of tooth decay. However, the 2024 Cochrane Review found fluoride may reduce decay by only a negligible amount.(3) Where is the benefit in the risk?
Research from personal testimony
References coming soon
Following are some of the findings from a two-year research and records requests project, part of which was presented in LB147 hearing testimony on March 12, 2025.
I set out in March, 2023, to determine how Nebraskans were handling the basics. With ever increasing data tracking required by state workers, to manage public health, fluoride treatment seemed to be a simple choice to investigate. Senators on the Legislature’s Health and Human Services Committee received the results of my research, and my efforts to lower the fluoride treatment level in Lincoln, stemming from a 2019 “aha” moment. Here is a portion of my results.
First a petition, signed by the state Public Health director, to align the outdated 1983 fluoride dosing regulation with the CDC’s 2015 recommendation. This revision became effective in January.
To reiterate, DHHS hadn’t updated its fluoride dosing regulation since 1983 despite the 2011 draft and 2015 final US Public Health Service recommendation to lower the fluoride level to 0.7 ppm due to rising fluorosis concerns. The state regulation remained between 0.8 and 1.5 ppm until January of this year. In comparison, 68% of water systems nationwide using systemic dosing reduced fluoride to 0.7 ppm within six months of the 2011 draft issue.
An excerpt from a 2009 study on fluorosis risk, from the Journal of the American Dental Association, shows that the difference in decay prevalence between optimally and non-optimally fluoridated communities is negligible.(Ref) This provides a benchmark for missing state-level data that Dr. Debra Esser confirmed last year was not available.
Table 2a and 2b are summaries comparing results of the Nebraska Oral Health Surveillance reports with the National Health and Nutrition Examination Surveys for the period 1999 to 2022.(Ref)(Ref) The results are mixed with some measures showing increased decay while others suggest reduced decay associated with increased sealant use.
Table shows the 75% increase, from $5,500 to roughly $9,600, in the total per member cost for Medicaid and CHIP since 2000. What portion of this increase is assigned to oral health, as described by Dr. Esser last year as the most common chronic medical condition?(Ref)
These results appear to refute the claims that systemic fluoride dosing reduces tooth decay by 25% and thereby reduces Medicaid costs. They also suggest the limited effectiveness of managing public health with data.
Finally, for Lincoln, Figure 1 and Table 4 compare fluoride treatment goals and testing levels for Lincoln with the 2015 CDC level and MUD-Omaha water quality reports for 2022 and 2023 both indicating opportunity to reduce Lincoln’s treatment by 10% or more.
Unlike MUD-Omaha, Lincoln’s water has been treated at 0.88 ppm with the city increasing the level to 0.94 last August. Lincoln will spend $116,000 this year on the cheapest fluoride additive type, a pollution collection byproduct, that offsets industry hazardous waste disposal costs.(Ref)
To close, instead of managing dental health by systemic fluoride dosing and increasing the collection of data points, currently over 50, please consider improving self-reliance. Bring transparency and choice to policy and educational materials by including the benefits of nourishing traditions and by highlighting the impact of malnutrition on decay. Many parents would welcome the services of a biological dentist and learning to recognize and treat many dental conditions on their own.(Ref)(Ref)
References
(1)Berg J, et al. Evidence-based clinical recommendations regarding fluoride intake from reconstituted infant formula and enamel fluorosis: a report of the American Dental Association Council on Scientific Affairs. J Am Dent Assoc 2011;142:79-87.
(2) Clark MB, Slayton RL, AAP SECTION ON ORAL HEALTH. Fluoride Use in Caries Prevention in the Primary Care Setting. Pediatrics. 2020;146(6):e2020034637
(3) Iheozor-Ejiofor Z, Walsh T, Lewis SR, Riley P, Boyers D, Clarkson JE, Worthington HV, Glenny AM, O’Malley L. Water fluoridation for the prevention of dental caries. Cochrane Database Syst Rev. 2024 Oct 4;10(10):CD010856. doi: 10.1002/14651858.CD010856.pub3. PMID: 39362658; PMCID: PMC11449566.
(4) American Academy of Pediatric Dentistry. Policy on
use of fluoride. The Reference Manual of Pediatric Dentistry. Chicago, Ill.: American Academy of Pediatric Dentistry; 2024:101-3
(5) American Academy of Pediatrics. Where We Stand: Fluoride Supplements. Retrieved 3/28/2025